RPM Manual
The practical 2026 guide to device rules, day thresholds, management time, and audit defensibility for Remote Patient Monitoring.
Read the RPM Guide →CMS has fused APCM eligibility, practitioner attribution, and continuity into a single monthly operating system--billing without that coherence now creates denial and audit exposure.
This is an operational guide grounded in public CMS materials--not legal advice. Confirm billing decisions with your MAC and current CMS guidance.
Eligibility, attribution, and continuity must reconcile inside the same billing month--CMS is paying for longitudinal ownership, not isolated events.
Billing APCM without month-specific attribution integrity, an active care plan, and continuity evidence bakes denials and audit exposure into your model.
APCM is Medicare’s monthly payment model for longitudinal, team-based primary care. It is built around continuity, access, care planning, coordination, and population-level management as part of ongoing responsibility for a panel. ([CMS][1])
CMS’s 2026 moves make the “one system” point concrete:
Result: eligibility, attribution, and continuity cannot be separated operationally--they must reconcile inside each billing month.
APCM billing is defensible only when eligibility, practitioner attribution, and continuity evidence reconcile within the same billing month--because CMS is explicitly aligning APCM payment, behavioral add-ons, and assignment logic around longitudinal primary care ownership. ([CMS][1])
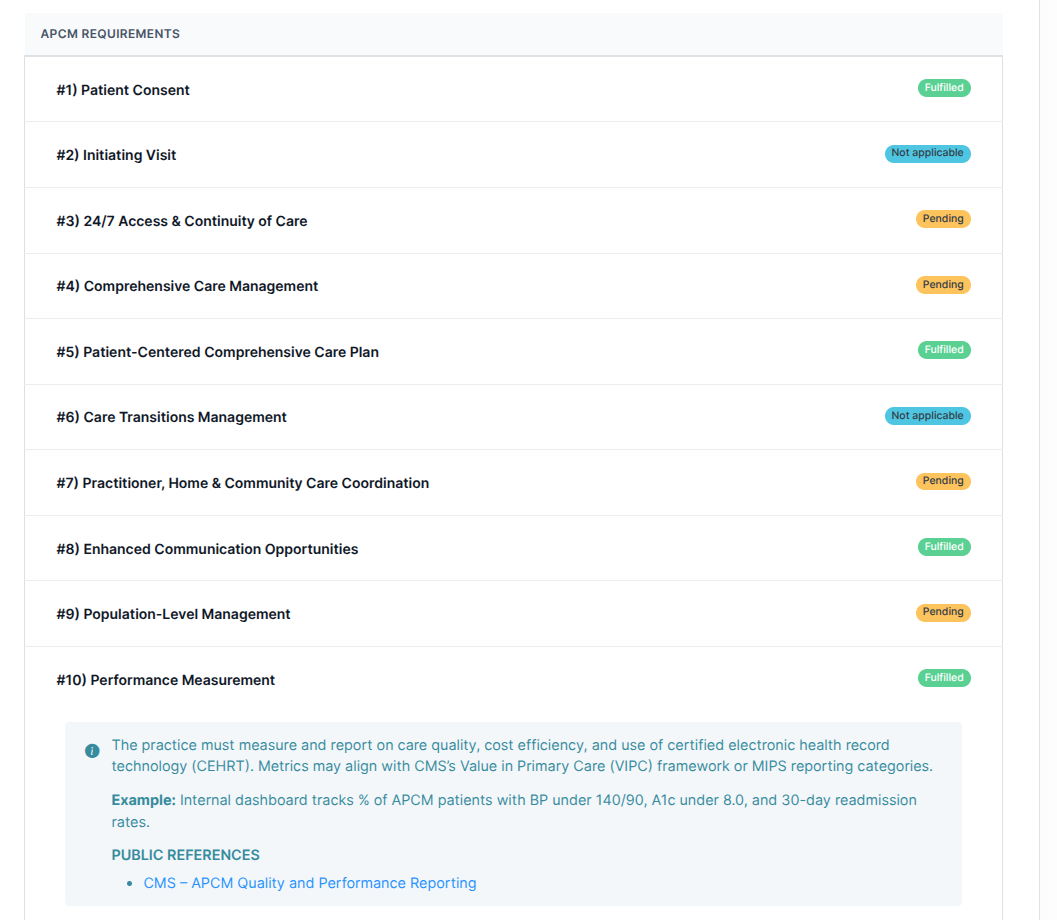
APCM is not a static enrollment flag. CMS frames APCM as a monthly service with defined requirements: consent, initiating visit logic (with exceptions), 24/7 access and continuity expectations, a comprehensive care plan, care transitions, coordination, enhanced communication, population-level management, and performance measurement. ([CMS][1])
Attribution answers which clinician/team is accountable for ongoing primary care management. CMS now counts APCM + BHI/CoCM add-ons as primary-care services for SSP beneficiary assignment, making attribution a payment and quality construct rather than a marketing roster. ([CMS][3])
Continuity is baked into APCM requirements: the ability to schedule successive routine appointments with a designated team member, 24/7 access for urgent needs, and longitudinal management. ([CMS][1])
CMS expects a patient-centered comprehensive care plan as part of APCM. ([CMS][4]) It is the simplest defensible continuity artifact: the longitudinal spine auditors understand.
Low readiness means your claims assert longitudinal management that your documentation cannot prove.
Patients stay on panels for months with minimal longitudinal documentation or care-plan maintenance.
Consent is collected once; APCM is billed repeatedly without month-specific evidence of APCM service elements.
Care plans exist but are treated as onboarding paperwork instead of living artifacts.
BH integration or monitoring activity is not clearly tied to the attributed practitioner, the APCM month, or the maintained plan.
BH add-ons are delegated to different clinicians or external teams, making the same practitioner/same month rule hard to satisfy. ([CMS][2])
Audits collapse complex reality into a simple question: Does the record support what the claim asserts, in the time period billed, under the responsible clinician?
OIG scrutiny of longitudinal billing (e.g., CCM overpayments; RPM oversight signals) shows enforcement follows expansion. ([Office of Inspector General][5])
You need month-specific evidence of review/management. A lightweight “reviewed and remains appropriate” attestation tied to the plan preserves time-period integrity.
Document outreach attempts, coordination actions, and plan review decisions. Attribution means responsibility even when the patient is quiet.
Only if explicitly anchored to the APCM plan-of-care and month-specific practitioner responsibility. Keep streams separate to avoid double-counting, but link monitoring artifacts to the APCM plan.
Snapshot attribution for billing periods so you can show responsible clinician/team as-of the APCM month for auditability.
The direction: claims-level coherence--services must hang together as a longitudinal model, not isolated billing events.
CMS is moving from reimbursing measurable tasks to reimbursing longitudinal accountability and integrating behavioral health into primary care ownership.
Result: claims and documentation stay coherent--eligibility, attribution, and continuity reconcile before submission.
Consent, initiating-visit logic for new patients (with defined exceptions), 24/7 access and continuity expectations, comprehensive care management, a patient-centered care plan, care transitions, coordination, enhanced communication, population-level management, and performance measurement. ([CMS][1])
You need month-specific evidence of ongoing management. A lightweight plan review/attestation can be sufficient when no substantive edits are needed because it preserves time-period integrity.
Yes. CMS finalized optional BH add-on codes for APCM. They must be billed in the same month by the same practitioner as the APCM base code. ([CMS][2], [CMS][6])
Same practitioner, same month as the APCM base code. They are designed to sit inside the primary care ownership model, not float independently. ([CMS][2])
CMS is aligning the definition of primary care services for SSP assignment with PFS payment changes, including APCM + BHI/CoCM add-ons. That ties APCM+BHI/CoCM activity to attribution mechanics beyond fee-for-service billing. ([CMS][3])
APCM is team-based, but documentation must support practitioner accountability for longitudinal management and APCM requirements. Capture explicit review/attestation and plan-of-care responsibility in the billed month. ([CMS][1])
Virtual direct supervision clarifies how immediate availability is satisfied for services requiring direct supervision; it does not expand who can do the work or what counts. ([CMS][6])
At minimum: consent record; initiating visit logic; attribution snapshot per month; care-plan versioning or monthly review attestation; evidence of access/continuity processes; and structured care-coordination events mapped to the plan.
While most platforms simply record what happened, FairPath actively runs the program. It continuously monitors every patient, staff action, and billing rule across CCM, RPM, RTM, and APCM, intervening immediately when a requirement is missed.
This allows you to scale your own program without losing quality, breaking trust with physicians, or losing control of your revenue. We provide the precision of an automated medical director without the chaos.
FairPath is built on operational work, not theory. We publish the playbooks and checklists we use to keep programs compliant and profitable. Use them whether you run FairPath or not.
Browse the Expert Library →The practical 2026 guide to device rules, day thresholds, management time, and audit defensibility for Remote Patient Monitoring.
Read the RPM Guide →How to run Remote Therapeutic Monitoring for MSK, respiratory, and CBT workflows with the correct 9897x and 9898x rules.
Read the RTM Guide →Calendar-month operations for CCM: consent, initiating visit, care plan requirements, time counting, and concurrency rules.
Read the CCM Guide →The operator blueprint for Advanced Primary Care Management: eligibility, G0556–G0558 tiers, and monthly execution.
Read the APCM Playbook →