RPM Manual
The practical 2026 guide to device rules, day thresholds, management time, and audit defensibility for Remote Patient Monitoring.
Read the RPM Guide →A survival guide for APCM, CCM, and Vendor Models under the new restrictions.
How to use this page: Use as a planning guide, not legal advice. Confirm coverage with your specific UHC contracts.
Effective January 1, 2026, UnitedHealthcare (UHC) will:
UnitedHealthcare’s December 2025 Medical Policy Update Bulletins and related documents:
This resource explains:
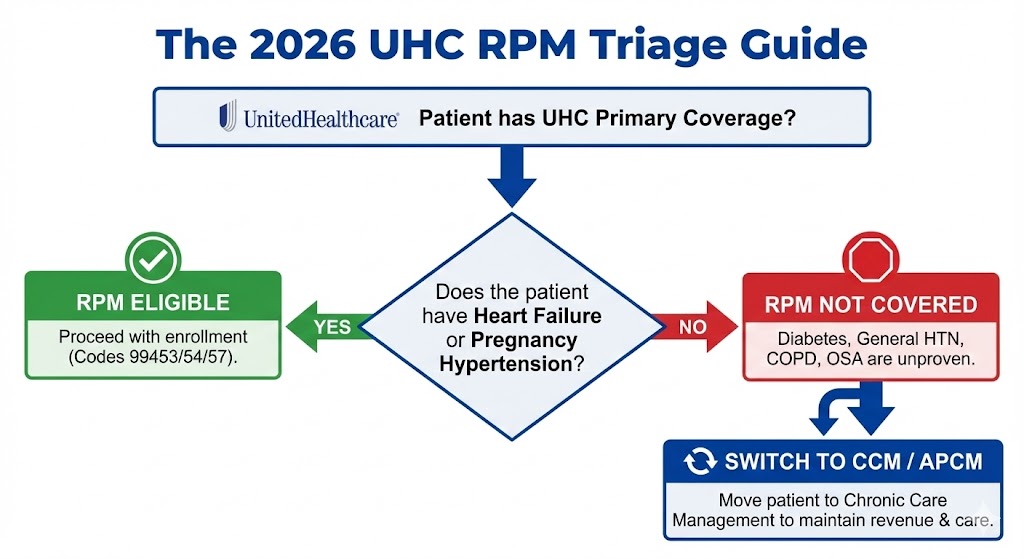
From January 1, 2026, UnitedHealthcare will pay for Remote Physiologic Monitoring only in narrowly defined cases (heart failure and hypertensive disorders of pregnancy) and will treat RPM as unproven/not medically necessary for most other conditions. No new 2026 UHC medical-policy bulletins were issued for RTM, CCM, or APCM.
In the December 2025 Medical Policy Update Bulletins, UHC lists:
The “quick view” summaries in these bulletins:
However, the full Commercial policy text is consistent with the Surest bulletin: RPM is medically necessary only for HF and HDP; all other uses are considered unproven and not medically necessary.
The Surest Medical Policy Update Bulletin (October 2025) provides the most detailed view:
Coverage rationale:
The Commercial full bulletin replicates this rationale, and UHC/industry commentary confirm it applies broadly across UHC product lines.
The general Community Plan Medical Policy Update Bulletin:
State-specific bulletins:
While each state Medicaid plan has its own nuances, the broader messaging and published policies strongly indicate UHC’s Medicaid RPM coverage will track the HF/HDP limitation.
The West Benefit Interpretation bulletin:
Across the December 2025 UHC bulletins:
This does not mean:
For your planning purposes:
If your practice or vendor bills UHC for RPM in 2026, think in terms of “clear yes” and “clear no.”
RPM is covered, proven, and medically necessary when:
And when the clinical and documentation requirements of the policy are met (device, monitoring period, management, etc.).
RPM is explicitly unproven/not medically necessary for indications including, but not limited to:
Even if RPM has been reimbursed under UHC in the past for these conditions, the 2026 policy change draws a bright line: future RPM claims for these indications are not covered.
UHC has clarified in media statements that:
Practically:
A separate item in the Community Plan of Pennsylvania bulletin addresses an external continuous pulmonary fluid monitoring system, where:
The 2026 update:
Important point:
Any RPM vendor whose business model relies heavily on:
faces a major problem:
If a vendor model is “UHC-heavy” in these categories, expect:
If your practice:
then:
The risk is especially high if:
UHC’s RPM stance combined with no changes to CCM/APCM in these bulletins suggests:
For your strategy:
Here’s a practical “pre-2026” checklist if UHC is a major payer for your panel:
If UHC is a meaningful payer for your practice and you’re reconsidering your remote-care strategy, take control of your panel now.
Read our full guide on CMS’ 2025–26 RPM & APCM rules and how to transition in-house.
Open the APCM/RPM GuideIf you lose UHC revenue, can you afford your vendor? Run the numbers instantly.
Use the Vendor Profit AnalyzerWorried about OIG or payer reviews? Download the 2026 Audit Survival Checklist.
Get the Audit ChecklistUHC’s 2026 RPM changes do not exist in a vacuum. They line up with three broader trends:
From FairPath’s standpoint, UHC’s RPM move is a live example of the thesis behind this product:
Reading the policy is one thing. Enforcing it across 2,000 patients is another. In FairPath, our Payer Ontology now reflects the 2026 UHC restrictions and automatically cross-references Payer (UHC), Diagnosis (I10 vs I50.9), and Program (RPM) so teams know where RPM is and is not covered.
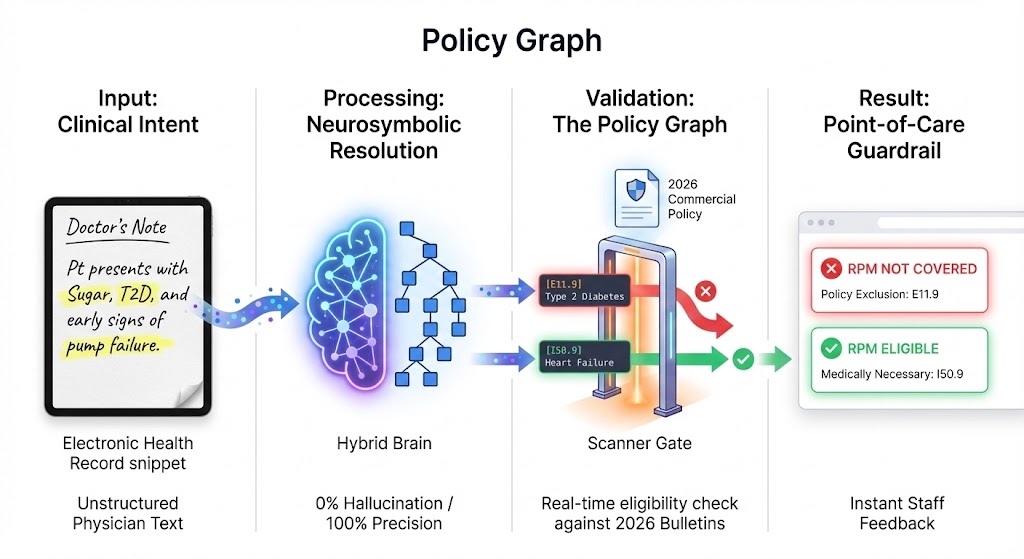
Result: you get an instant “Not Covered” flag for ineligible patients before staff time is spent enrolling them.
No, but under UHC it is now narrowly defined. RPM is still covered for heart failure and hypertensive disorders of pregnancy, and possibly for specific technologies under other policies. However, UHC has taken the position that RPM is unproven for many chronic conditions (like diabetes and general hypertension) that RPM vendors previously targeted.
You can clinically monitor these patients however you and the patient decide, but under UHC’s 2026 medical policy, RPM professional service codes are considered unproven/not medically necessary for those indications. That means you should not expect RPM claims for these conditions to be payable under UHC.
In many cases, yes, as devices under members’ benefit plans or DME benefits. UHC has signaled that it may still cover home monitoring devices where appropriate. What’s changing is not the device benefit itself, but the separate RPM professional service codes for many conditions.
Based on the December 2025 bulletins, UHC did not issue new RTM medical policies for 2026. That doesn’t necessarily mean there are no RTM policies; it simply means there were no new RTM updates in this specific bulletin set. You should review UHC’s reimbursement policies and specific RTM guidance separately.
The December 2025 medical-policy bulletins did not introduce new APCM or CCM policies. Those services continue to be governed by existing rules and reimbursement policies. Strategically, UHC’s narrowing of RPM and the federal expansion of APCM/CCM suggest that care-management programs (APCM, CCM, BH-Collaborative Care) are where payers expect continuous care to live, with RPM as a narrower adjunct.
You should plan your RPM/APCM strategy so it’s resilient across payers, not designed only for one.
For UHC in particular, RPM should move from being a broad chronic-disease tool to a narrow intervention for heart failure and hypertensive disorders of pregnancy. For the rest of your chronic Medicare and commercial population, consider an APCM/CCM-first model: treat APCM (or equivalent care-management constructs) as the base for continuous care, and use RPM only where payers still cover it and where real-time data changes management. That approach is more aligned with CMS’s direction and more resilient if other payers follow UHC’s lead.
Below is a non-exhaustive list of primary and secondary sources used to build this summary. You should consult these directly before making policy decisions.
(All list “Remote Physiologic Monitoring (RPM)” as a new medical policy effective Jan 1, 2026.)
While most platforms simply record what happened, FairPath actively runs the program. It continuously monitors every patient, staff action, and billing rule across CCM, RPM, RTM, and APCM, intervening immediately when a requirement is missed.
This allows you to scale your own program without losing quality, breaking trust with physicians, or losing control of your revenue. We provide the precision of an automated medical director without the chaos.
FairPath is built on operational work, not theory. We publish the playbooks and checklists we use to keep programs compliant and profitable. Use them whether you run FairPath or not.
Browse the Expert Library →The practical 2026 guide to device rules, day thresholds, management time, and audit defensibility for Remote Patient Monitoring.
Read the RPM Guide →How to run Remote Therapeutic Monitoring for MSK, respiratory, and CBT workflows with the correct 9897x and 9898x rules.
Read the RTM Guide →Calendar-month operations for CCM: consent, initiating visit, care plan requirements, time counting, and concurrency rules.
Read the CCM Guide →The operator blueprint for Advanced Primary Care Management: eligibility, G0556–G0558 tiers, and monthly execution.
Read the APCM Playbook →