RPM Manual
The practical 2026 guide to device rules, day thresholds, management time, and audit defensibility for Remote Patient Monitoring.
Read the RPM Guide →Revenue-share vendors drain your margin while you hold 100% of the audit and legal liability. FairPath is the compliance-first operating system that lets your practice run RPM, APCM, RTM, and CCM on a single spine.
Updated with the latest codes and guidance for 2026 for RPM/RTM/APCM/CCM.
Who this is for
"If you want remote care to behave like part of your core practice--not a side hustle--you’re in the right place."
See exactly how much revenue you lose to vendor fees vs. FairPath's flat pricing.
Program Design
Before you think about vendors, rev-share, software, or staffing, it helps to define what “good” looks like. In 2026, healthy RPM programs are targeted, layered on top of broader management models like APCM and CCM, and measured by outcomes and workload--not just codes.
RPM is not simply “for everyone with hypertension.” Robust programs start with a structured qualification process:
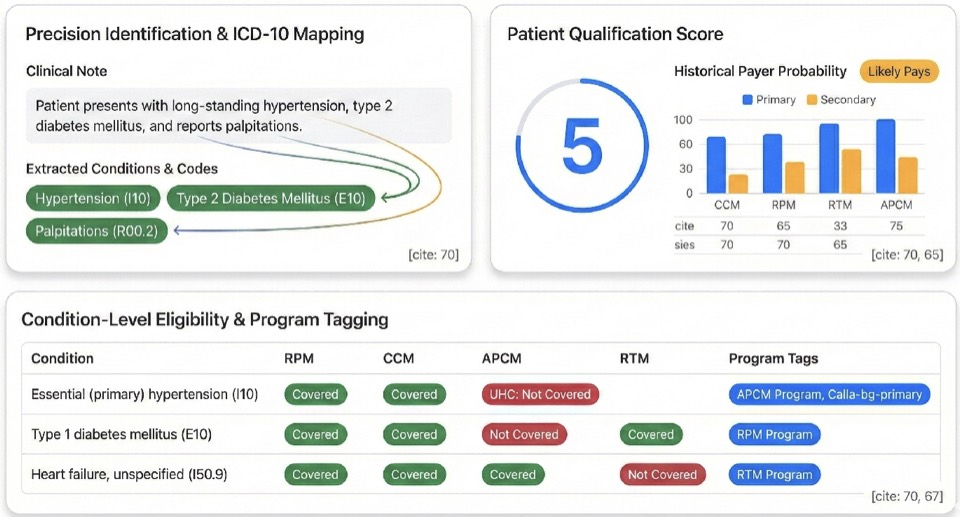
FairPath’s 1–5 Eligibility Score is one example: it consolidates diagnosis, utilization, and payment patterns into a simple, panel‑wide view of who truly fits RPM, APCM, CCM, or some combination.
The most stable clinics treat RPM as a layer on top of a broader remote‑care spine:
RPM‑only strategies are fragile. RPM on top of APCM/CCM is resilient and better aligned with where payers and regulators are going.
Healthy programs optimize for:
And they do this while minimizing manual tracking and multiple portals, keeping staff focused on clinically meaningful work instead of “threshold management.”
FairPath was built to embody these principles: structured eligibility scoring, an APCM‑first design with RPM/RTM/CCM layered on top, and queues that direct your team to the few tasks that matter rather than chasing raw code volume.
One operating system for APCM, RPM, CCM, and RTM—from eligibility and onboarding to billing, compliance, and scale.
The most common objection to bringing RPM, APCM, RTM, or CCM in-house is bandwidth. FairPath’s queue-based architecture lets you work as little or as much as you want: whether you have 30 minutes a day or a dedicated team, the system prioritizes work so you never waste time, eliminate repetitive manual steps, and keep the focus on patient health first.
Most practices struggle with remote care because they improvise who to enroll. FairPath replaces guesswork with structured, scalable decision-making. We turn the chaos of payer rules, diagnosis codes, and payment history into a single 1–5 Qualification Score for each patient, so you see exactly who is viable for APCM, RPM, CCM, or RTM without manual chart review.
Predictive payer scoring built from your own data. FairPath ingests your 835 (ERA) payment files to learn from your actual claims history, predicting which payers and codes will reimburse and filtering out high-denial plans before you ever start enrollment.
One dashboard maps diagnoses to programs (e.g., HTN, Diabetes, COPD, CKD → APCM, RPM, CCM), showing which chronic conditions qualify for which programs in a single, simple table tuned to your clinical policies.
We automatically update the logic for CMS rules, insurance policy shifts, and ICD code changes (including ICD-11). Your eligibility scores and panel design never go stale as regulations evolve.
The Operational Shift: You never waste time chasing ineligible patients. Every enrollment minute is directed at a clinically appropriate, reimbursable candidate.
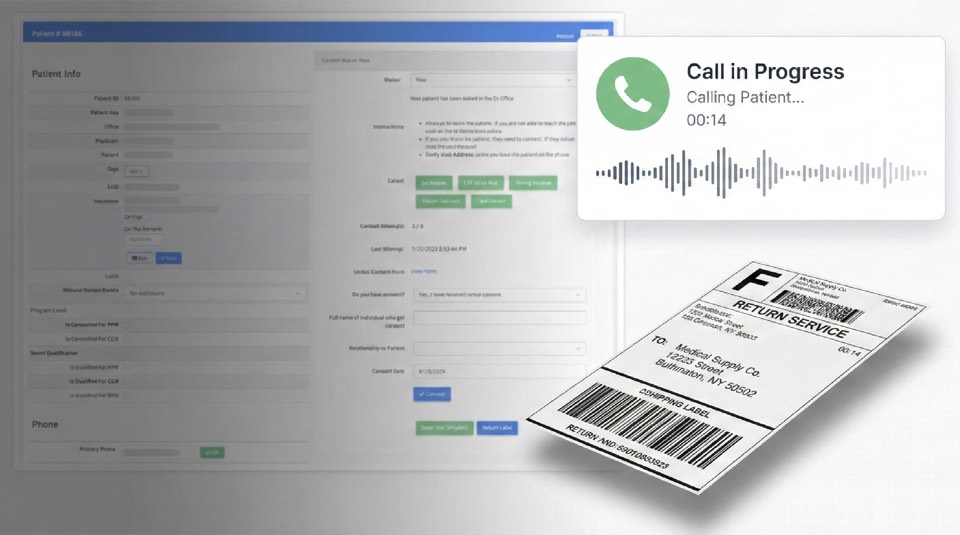
Move from “ad-hoc notes” to a structured, browser-based Onboarding Module. FairPath unifies communication, documentation, and hardware logistics in a single flow—staff call patients from the browser, capture verbal consent, and assign device serial numbers without spreadsheets.
Call patients directly from the browser using built-in onboarding scripts. FairPath delivers training materials and automatically records and transcribes verbal consent to the chart while simultaneously kicking off downstream logistics.
Track serial numbers and assignments in one place—no separate trackers. Generate return shipping labels instantly and prevent billing for inactive or lost devices.
Send templated patient letters, save signed forms, and archive all training records in a single, audit-ready profile.
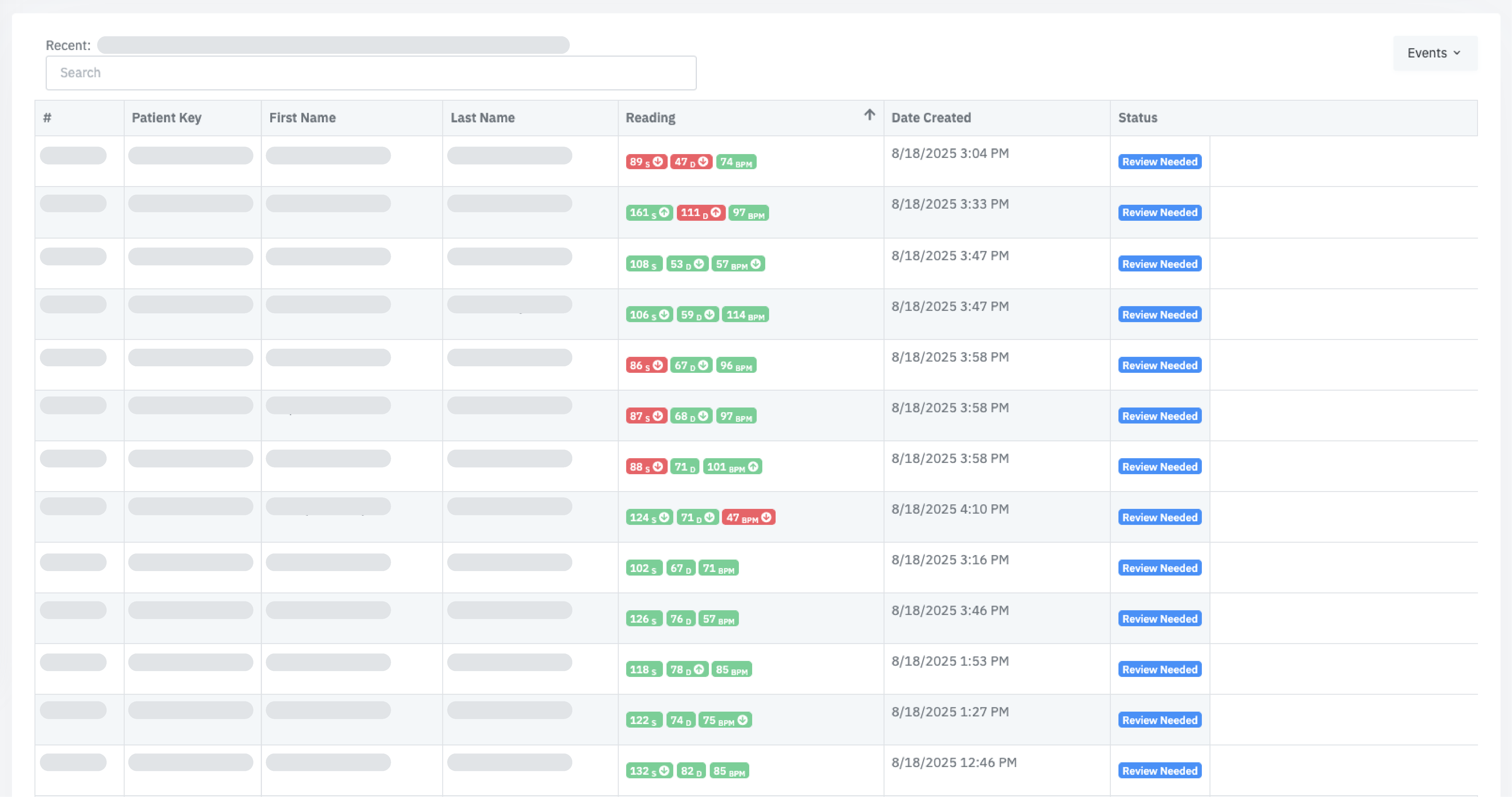
Your operations team lives in PriorityQ and ReviewQ—consolidated queues that sort work by urgency, clinical risk, and code completion. Instead of reviewing every reading, your staff works from a single queue of exceptions: critical vitals, worsening trends, and “no data” patterns. The same interface works for 50 or 5,000 patients; only the queue length changes, with Amy (AI) handling routine nudges and troubleshooting in the background.
Consolidates new readings, APCM service tasks, “Device Problem” events, and exception alerts into one prioritized list so every click advances both patient outcomes and billing progress.
Calls and texts are initiated from the queue. Every interaction is timestamped and attached to the patient record, feeding BillingQ and your audit trail automatically.
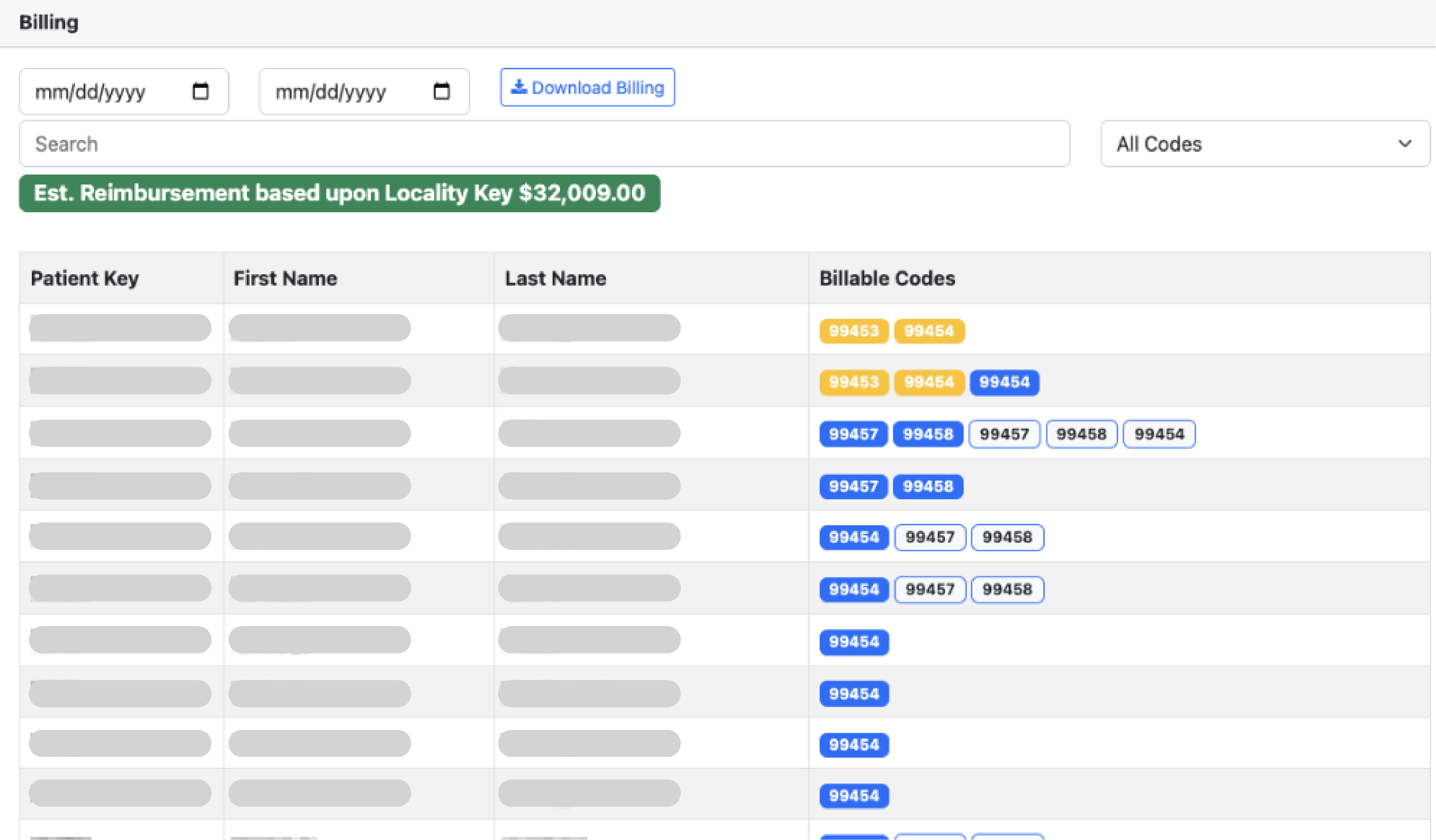
Make “Compliance-as-Code” real. BillingQ treats compliance as a systems problem, not a training problem—encoding the rules so risky claims never make it to your billing team.
Don't reinvent the wheel. FairPath includes embedded operational procedures for enrollment, review, and QA, refined over millions of patient interactions.
The same operating model works for 100 patients or 10,000+. Queue-based workflows mean you scale by adding roles, not by rewriting software.
Structured care pathways, AI-assisted drafting, and patient engagement that keeps clinicians in control—even as you scale from a few dozen patients to a multi-thousand panel.
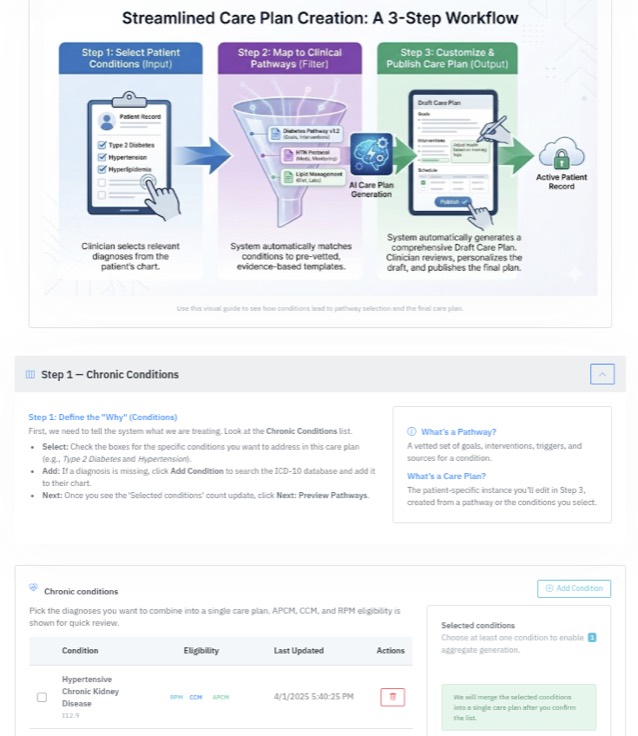
Remote care fails without a roadmap. FairPath provides Ontology-Driven Pathway Schemas that act as the clinical blueprint for your program—ensuring every patient receives consistent, high-quality care. Developed in partnership with leading clinicians and refined over millions of patient interactions.
Amy (AI) analyzes patient history and comorbidities to draft a comprehensive care plan for you. She suggests goals, phases, and interventions based on your clinical guidelines—all within a secure, HIPAA-compliant environment.
Draw from our library of best-practice schemas (HTN, Diabetes, COPD), or encode your own proprietary protocols.
Stop juggling separate plans. Create a single CarePlan that manages multiple chronic conditions at once. The system links documented activities to program requirements and shows progress toward common thresholds; payer rules vary and the practice remains responsible for coding.
Track every development. FairPath audits every change to the care plan, creating an immutable history of patient progress and provider decision-making.
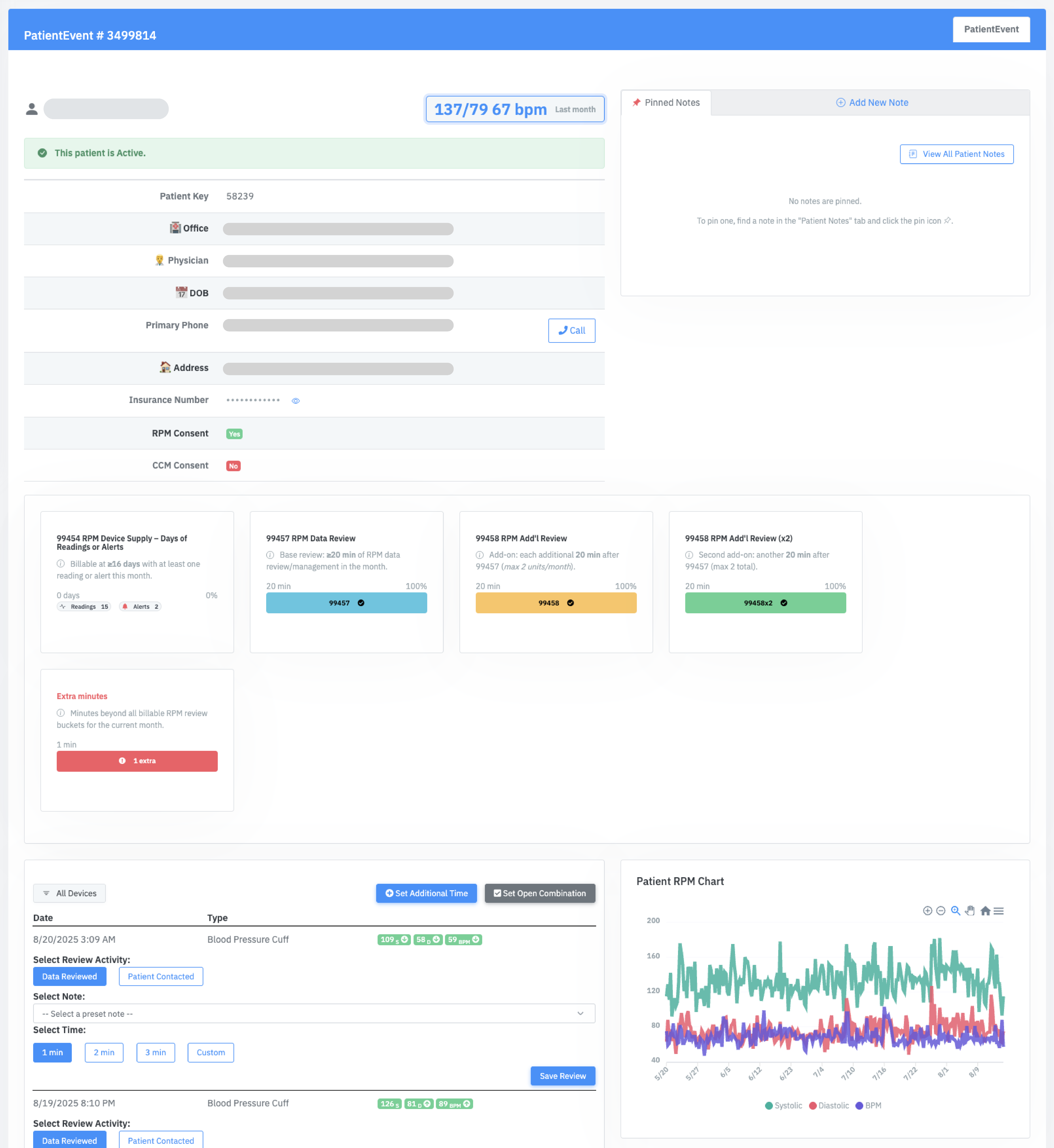
The Priority Q puts the most important patients in front of you first. Instead of reviewing every reading or bouncing between charts, clinicians work from a single queue of exceptions—critical vitals, worsening trends, and “no data” patterns. AI evaluates incoming readings in real time so you decide how hands-on you want to be, and the software absorbs the rest.
Critical alerts jump to the top. Scheduled follow-ups for CCM and APCM appear automatically when due. Filter by event type or let the AI decide what's next so your effort is defined by clinical need, not panel size.
Watch billing codes track in real-time. As you log time or complete tasks, progress bars fill up instantly so you know exactly when thresholds (like CCM 20 mins) are met.
Call or text patients directly from the chart or queue. Every attempt is automatically logged to the audit trail and contributes to time tracking.
Stop typing. FairPath automatically transcribes and summarizes every phone call. You can also dictate your own clinical notes. Both the original audio and transcript are saved in a HIPAA-compliant archive.
Amy (AI) is an embedded capability of FairPath—not a separate product. She handles routine friction so your clinicians can focus on complex care: sending nudges to keep patients on track for RPM requirements (like 16 days of readings), troubleshooting connectivity, and delivering structured symptom surveys via text or voice.

Walks patients through fixing connectivity issues to keep data flowing.

Reminds patients to take readings or complete APCM elements.

Collects structured symptom data and answers common questions.

Recognizes clinical risk and hands off to human staff with context.
The Operational Shift: You choose how little or how much to personally touch; FairPath ensures that whatever reaches your staff is worth their time, defined by exceptions rather than panel size.
Backed by SemDB and OGAR guardrails to ensure HIPAA compliance and minimize hallucinations.
When RPM is managed correctly--as part of a thoughtful remote‑care stack--the clinical lift is significant. In a controlled study of 192 chronic‑care patients, structured monitoring delivered:
Out‑of‑bounds readings dropped from 59% to 42% in just 90 days.
Daily reading frequency increased by 22% as patients engaged with the feedback loop.
Reduction in Out‑of‑Bounds Readings
Due Diligence Briefing
Remote care programs can be run internally or outsourced to a "full-service" vendor. While vendors initially appeared to solve logistical problems, a clear set of structural risks has emerged. The market is actively shifting away from these high-volume "RPM Factories" toward panel-based models like APCM. Before signing or renewing, evaluate your program against these three critical pillars.
Vendor models are often built on "revenue share," but in practice, they capture the majority of the program's value while leaving you with the denial risk.
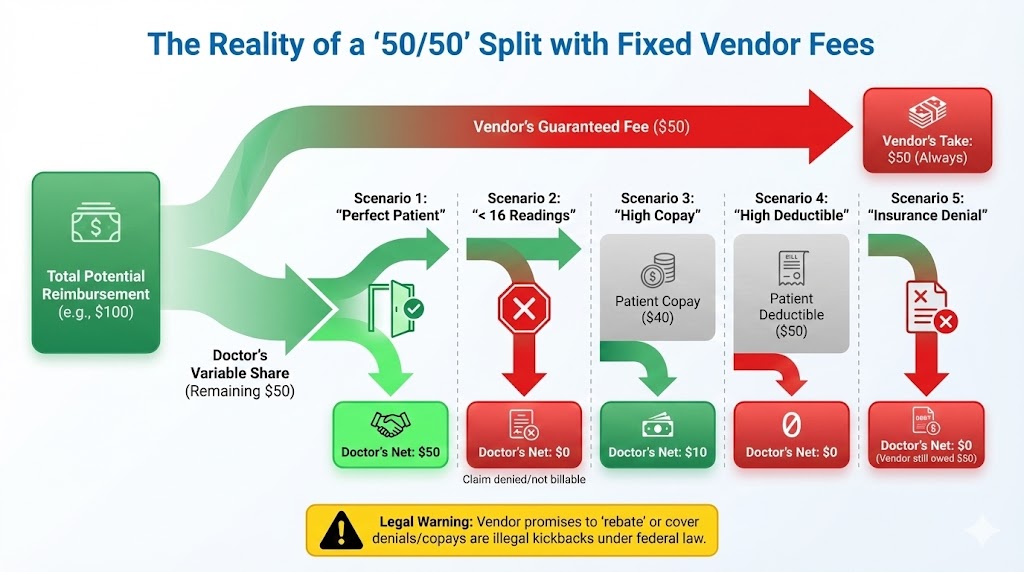
When you add device charges, shipping, and administrative fees to a standard revenue share, it is common to see vendors consuming 50–70% of total program revenue.
Persistent Fees: You often owe fees even if patients miss the 16-day threshold or claims are denied.
Device Liability: Hardware costs frequently stay with the practice if devices are lost or unreturned.
“I don’t care if the doctor makes money.”
-- CEO of a leading remote care company, describing their business model
Key Question: What is your realistic net RPM margin after all vendor-related costs across diverse real-world scenarios?
When vendor income scales with enrolled patients and billed codes, the incentive tilts toward volume: broad enrollment of "on paper" candidates and a tendency to "stretch" time rules.
Concerns about volume-based payments tied to federal program business.
FCA Risk: If billing systems systematically overstate time, components, or medical necessity.
The Market Reality: Oversight bodies are responding. The OIG found substantial non-compliance in high-volume programs, and payers like UHC (2026 Policy) are narrowing coverage criteria in direct response. High-volume, vendor-heavy programs now operate under maximum scrutiny.
A contract can be technically defensible on paper and still push behavior toward the edge of what regulators will tolerate. Ultimately, your NPI is on the claim.
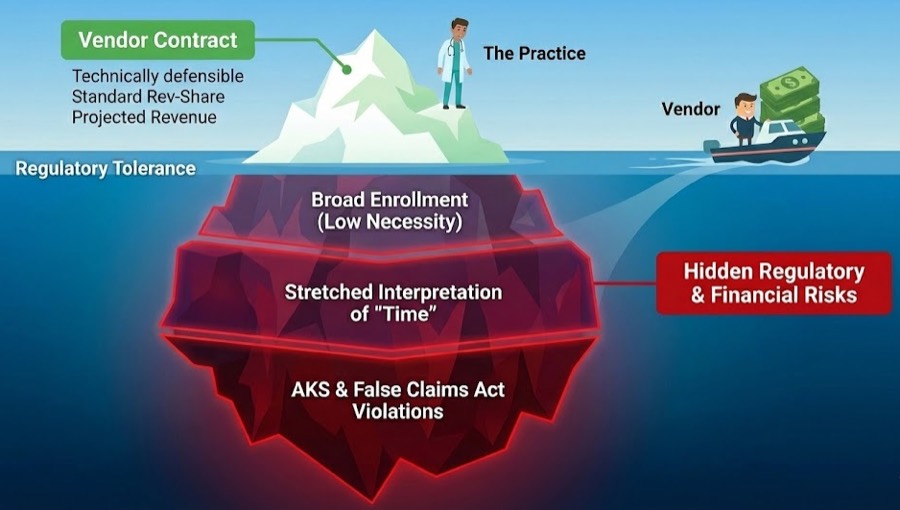
Outsourcing creates a "Black Box" around your data and locks you into a device-centric model just as the market shifts toward comprehensive care (APCM).

Vendor models optimized for RPM hardware margins align poorly with an APCM-first strategy, where RPM is used selectively as a clinical tool rather than a volume driver.
Vendors often prioritize "clean" claims, leading to the exclusion of complex patients who need care most. Furthermore, because outreach comes from the vendor but looks like it comes from you, aggressive reminders or scripted calls damage your brand.
In many vendor models, the complete audit trail lives in their portal. Full, structured exports can be difficult or costly to obtain, complicating any future transition.
CMS is actively incentivizing panel-based models like APCM. These models reward ongoing primary care rather than device quotas and naturally align with in-house teams--not with external "RPM factories" taking a percentage of reimbursement.
Don't sign a "full-service" vendor agreement until you have clear answers to these six questions:
What is our realistic net RPM margin after accounting for all vendor costs, denials, and lost devices?
How do you ensure we receive our revenue split without violating the Anti-Kickback Statute?
Are you willing to assume legal and financial risk if CMS audits and claws back reimbursements?
How do you deal with patients who have co-pays? Or patients on Medicaid?
Can we download a complete, structured export of our data today without a fee?
What is the specific cost to exit this contract before the 1-year mark?
OIG’s RPM findings and payer policy changes are not abstract. They are direct responses to the high‑volume, low‑documentation patterns that vendor‑driven models created.
Regulators are targeting "device quotas" and high-volume billing without clinical context.
CMS is actively incentivizing panel-based management models like Advanced Primary Care Management (APCM).
FAQ
These FAQs focus on how a modern, in‑house RPM/APCM/RTM/CCM stack works on FairPath--and how to think about vendors if you’re currently using one.
No, and this is a critical risk. Payer policies are tightening. UnitedHealthcare’s 2026 policy states RPM is only “necessary” for heart failure and hypertensive disorders of pregnancy, meaning RPM for other common conditions can be denied.
This is why relying only on RPM is dangerous. FairPath integrates Advanced Primary Care Management (APCM), a CMS‑approved program with stable, predictable revenue that isn’t diagnosis dependent. We help you build durable APCM revenue and layer RPM where it is both clinically appropriate and financially secure.
This is the “Vendor Trap.” That 50–70% rev‑share erases your margin.
The Math: You bill $100. They keep $70. You keep $30.
The FairPath Model: You bill $100. You pay a simple software fee. You keep the rest.
We stay transparent, while rev‑share vendors obscure true practice profit and push billing patterns that leave you holding the liability. FairPath provides the operating system; you keep the revenue you earn.
No. FairPath sits alongside your existing EMR. We integrate with your current workflows so your team doesn’t have to relearn everything or juggle another core system.
Stop trying to do it manually. FairPath’s Compliance‑as‑Code engine prevents bad claims before they are submitted by:
Your staff doesn’t have to memorize billing rules--our software already knows them.
Start by requesting two things: a complete patient data export and the exit fee. Vendors that resist either are signaling lock‑in.
We are the anti‑vendor. FairPath is built on 100% Data Sovereignty. From day one you have full access to patient lists, device logs, and claim history, and you can export them anytime. Use the RPM Vendor P&L Analyzer and our Exit Blueprint to understand both the economics and the operational path out.
You take back control. Rev‑share vendors often lock you into pricey hardware leases to create hidden margins.
FairPath is device‑agnostic. We integrate with low‑cost commodity hardware and support patient‑owned devices where appropriate so you can reduce overhead and keep the margin you earn--without making hardware a new point of lock‑in.
Payer policy will change, and it will be disruptive. UHC’s 2026 update proves RPM‑only programs sit on unstable ground.
FairPath is a multi‑program platform that centralizes RPM, RTM, CCM, and especially APCM. When payers tighten RPM, you can pivot to APCM instead of watching revenue collapse. Our goal is to keep your practice stable, diversified, and ready for whatever comes next. If you want to understand the APCM‑first model in detail, read our APCM‑First strategy guide →.
Plan on 60–90 days. We start by stabilizing your current panel, then run FairPath alongside your vendor so you can validate eligibility scoring, PriorityQ, and BillingQ against their work. Once the data and payouts match, we wind down the vendor contract--without forcing you to hire new staff.
Whether you are just exploring remote‑care options or actively evaluating a vendor, you don’t have to guess. See how FairPath would run your stack, and benchmark your current model against a software‑driven, APCM‑first approach.
The RPM Vendor P&L Analyzer takes "we’re probably getting ripped off" and turns it into hard numbers. Enter your vendor, patient count, and rev-share to see:
Not another vendor. The software you use to replace the vendor.
Runs APCM, RPM, CCM, and RTM on one integrated platform.
Eligibility scoring, Amy (AI Assistant), PriorityQ, and BillingQ automate the work.
Works alongside your EMR under your governance. Your data, always.
FairPath works alongside the EMR you already use:
FairPath is built on operational work, not theory. We publish the playbooks and checklists we use to keep programs compliant and profitable. Use them whether you run FairPath or not.
Browse the Expert Library →The practical 2026 guide to device rules, day thresholds, management time, and audit defensibility for Remote Patient Monitoring.
Read the RPM Guide →How to run Remote Therapeutic Monitoring for MSK, respiratory, and CBT workflows with the correct 9897x and 9898x rules.
Read the RTM Guide →Calendar-month operations for CCM: consent, initiating visit, care plan requirements, time counting, and concurrency rules.
Read the CCM Guide →The operator blueprint for Advanced Primary Care Management: eligibility, G0556–G0558 tiers, and monthly execution.
Read the APCM Playbook →